Notice
|
2022
09.09
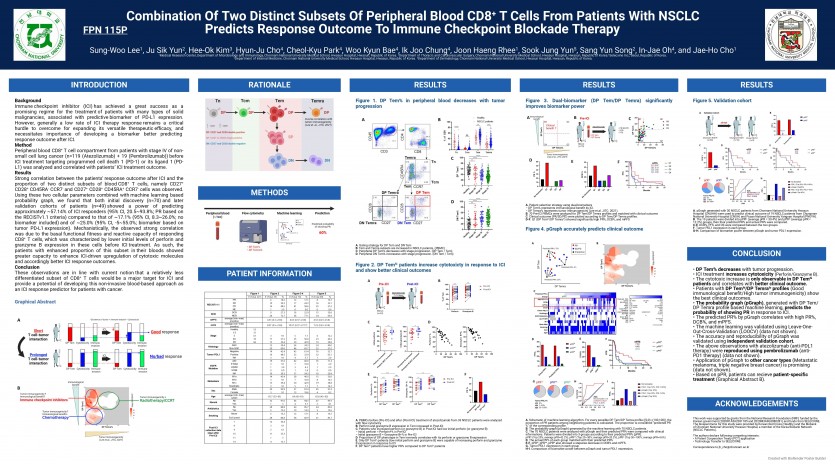
Events [POSTER] ESMO 2022: Combination Of Two Distinct Subsets Of Peripheral Blood CD8+ T Cells From Patients With NSCLC Predicts Response Outcome To Immune Checkpoint Blockade Therapy Poster submission
|
|---|
|
ESMO 2022: 동반진단 Poster submission
<Introduction>
Background Immune checkpoint inhibitor (ICI) has achieved a great success as a promising regime for the treatment of patients with many types of solid malignancies, associated with predictive biomarker of PD-L1 expression. However, generally a low rate of ICI therapy response remains a critical hurdle to overcome for expanding its versatile therapeutic efficacy, and necessitates importance of developing a biomarker better predicting response outcome after ICI. Method Peripheral blood CD8+ T cell compartment from patients with stage IV of nonsmall cell lung cancer (n=119 (Atezolizumab) + 19 (Pembrolizumab)) before ICI treatment targeting programmed cell death 1 (PD-1) or its ligand 1 (PDL1) was analyzed and correlated with patients’ ICI treatment outcome. Results Strong correlation between the patients' response outcome after ICI and the proportion of two distinct subsets of blood CD8+ T cells, namely CD27+ CD28+ CD45RA- CCR7- and CD27+ CD28+ CD45RA+ CCR7- cells was observed. Using these two cellular parameters combined with machine learning based probability graph, we found that both initial discovery (n=70) and later validation cohorts of patients (n=49) showed a power of predicting approximately ~57.14% of ICI responders (95% CI, 20.5~93.8%; PR based on the RECISTv1.1 criteria) compared to that of ~17.1% (95% CI, 8.3~26.0%; no biomarker included) and of ~25.0% (95% CI, -5~55.0%; biomarker based on tumor PD-L1 expression). Mechanistically, the observed strong correlation was due to the basal functional fitness and reactive capacity of responding CD8+ T cells, which was characterized by lower initial levels of perforin and granzyme B expression in these cells before ICI treatment. As such, the patients with enhanced proportion of this subset in their bloods showed greater capacity to enhance ICI-driven upregulation of cytotoxic molecules and accordingly better ICI response outcomes. Conclusion These observations are in line with current notion that a relatively less differentiated subset of CD8+ T cells would be a major target for ICI and provide a potential of developing this non-invasive blood-based approach as an ICI response predictor for patients with cancer.
|